>Corresponding Author : Karavdic K
>Article Type : Letter to the Editor
>Volume : 3 | Issue : 7
>Received Date : 04 Oct, 2023
>Accepted Date : 13 Oct, 2023
>Published Date : 17 Oct, 2023
>DOI : https://doi.org/10.54289/JCRMH2300132
>Citation : Firdus A, Karavdic K, Hadziosmanovic O, Cerovac A, Hrgovic Z, et al. (2023) Formation of Diagonal Gaps as Stress-Relieving Sites: Rethinking the Concept of Increment Splitting in Direct Occlusal Composite Restorations. J Case Rep Med Hist 3(7): doi https://doi.org/10.54289/JCRMH2300132
>Copyright : © 2023 Firdus A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Letter to the Editor | Open Access | Full Text
1Clinic for Pediatric Surgery, Clinic Center of University Sarajevo, Bosnia and Herzegovina
2Clinic for Urology, Clinic Center of University Sarajevo, Bosnia and Herzegovina
3General Hospital Tešanj, Bosnia and Herzegovina
4Institut for Pathology, Clinic Center of University Sarajevo, Bosnia and Herzegovina
*Corresponding author: Karavdic A, Clinic for Pediatric Surgery, Clinic Center of University Sarajevo, Bosnia and Herzegovina
Abstract
Bladder urothelial neoplasms are very rare in people in the first two decades of life. We presented our experience in the diagnosis and treatment of a fourteen-year-old adolescent girl with a tumor process on the urinary bladder.
Keywords: Girl; Urinary Bladder; Neoplasm
To the Editor,
Bladder urothelial neoplasms are very rare in people in the first two decades of life, only 0.1-0.4% [1]. Precisely because of the small number of cases, the prognosis of urothelial neoplasms of the urinary bladder is not sufficiently known, and there are no clear guidelines for postoperative monitoring and follow up. These are usually changes that are small in size, solitary, low-grade and non-invasive in the muscle layer of the bladder, and have minimal potential for local spread and recurrence [1,2].
In our case, we are presenting a fourteen-year-old adolescent girl who was referred by a pediatrician for surgery due to a tumor process on the urinary bladder. Three months ago, the patient had complaints in the form of pain at the lower abdomen, without a change in the color of her urine. The change in the urinary bladder was detected by an echosonographic examination. Magnetic resonance imaging of the urinary tract and cystoscopic examination were performed, which confirmed the ultrasound findings. Intraoperatively, a cauliflower-like tumor proliferation was verified above the left vesicoureteral orifice and was resected together with the intravesical portion of the vesicoureteral orifice, and its base and edges were cauterized (Figure 1,2).
Microscopic description: fragments of the bladder mucosa dominate in the examined sections, without a discernible muscle layer. One particle corresponds to tumor tissue, papillary structure, which is made of unfused, branched papillae, thin fibrovascular stands that are lined with hyperplastic transitional type epithelium whose cells are arranged in more than seven rows in some visual fields. There are foci with nucleomegaly of cells, sporadically prominent nucleoli, with low mitotic activity (3 mitoses in the complete tumor). Hyperplastic navicular cells can be seen on the surface of individual papillae. Proliferative index Ki-67 (approx. 15%). Tumor cells are located intraepithelially, without signs of invasion and fibrovascular scaffolds and deeper structures of the lamina propria of the bladder mucosa (Figure 3,4,5).
During the first year of follow-up, the three-month control laboratory findings as well as the urine cytology were normal. Control MRI, echo of the urotract and abdomen, and cystoscopy were normal (Figure 6,7).
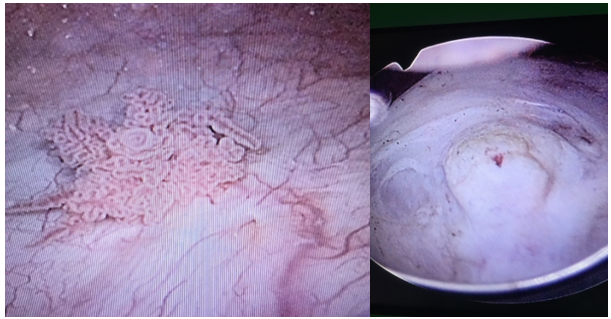
Figure 1,2 Intraoperative finding of PUNLMP
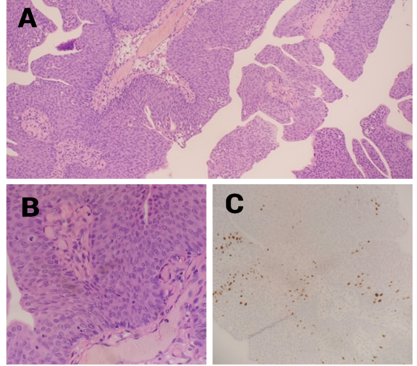
Figure 3,4,5 Patohistological finndings A. HE, x100, B. HE x400, C. Ki 67
Barrettini et al in their 14-year retrospective study analyzed 18 cases with urothelial neoplasms of the bladder, 8 of which were PUNLMP. Most patients had gross haemathuria, while the average size of the lesion was 16.7 mm. After an average follow-up of 5 years, a single case of recurrence or progression of the disease was not recorded [1]. Polat et al in their multicenter retrospective study analyzed 11 cases of bladder tumors, two of which were PUNLMP, with no recorded cases of disease recurrence [2].
PUNLMP in the general population has a recurrence of 9%, but in the same form of PUNLMP or in low-grade carcinoma without invasion, there were no cases of recurrence in high-grade form or invasive carcinoma during long-term follow-up [3]. In most cases, PUNLMP are solitary lesions located near the ureteral oriffice [4,5].
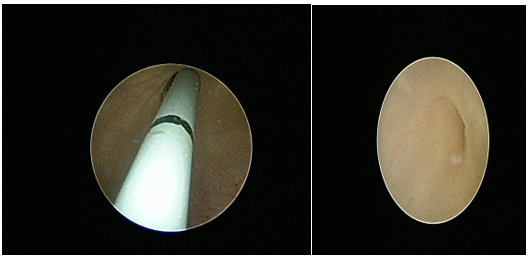
Figure 6,7 Control cystoscopy is satisfactory with no signs of recurrence
Umlauf et al and Park et al independently reported by two cases of PUNLMP with similar clinical picture, diagnosis and therapy as in our case, with the difference that all presented cases had gross haemathuria which was not present in our case [4,5].
PUNLMP is a rare neoplasm in children and adolescents, which is described in the literature through rare case reports and smaller case series, so additional multicenter international studies are needed to achieve clear guidelines for diagnosis and follow-up of patients with this diagnosis.
Ultrasound is a sufficient tool for the diagnosis of PUNLMP, while TURB is sufficient for the treatment of the lesion. Ultrasound and cystoscopic monitoring with gradually increasing intervals is recommended, while cytological analysis of urine is considered an insufficiently sensitive method for the detection of PUNLMP.
Compliance with ethical standards
Conflict of interest: The authors have nothing to disclose and no conflict of interest to declare. No funding source was involved in this study and there are no financial or other relationships that could be perceived to influence the manuscript.
Ethical approval: In our institution it is not required for case reports.
References
- Berrettini A, Castagnetti M, Salerno A, Nappo SG, Manzoni G, et al. (2015) Bladder urothelial neoplasms in pediatric age: experience at three tertiary centers. J Pediatr Urol. 11(1): 26.e1-25. [PubMed.]
- Polat H, Utangac MM, Gulpinar MT, Cift A, Erdogdu IH, et al. (2016) Urothelial neoplasm of the bladder in childhood and adolescence: a rare disease. Int Braz J Urol. 42(2): 242-246. [PubMed.]
- Maxwell JP, Wang C, Wiebe N, Yilmaz A, Trpkov K. (2015) Long-term outcome of primary Papillary Urothelial Neoplasm of Low Malignant Potential (PUNLMP) including PUNLMP with inverted growth. Diagn Pathol. 10: 3. [PubMed.]
- Umlauf VN, Coerdt W, Leuschner I, Schröder A, Stein R, et al. (2015) How to Name Papillary Tumors of the Bladder in Children: Transitional Cell Carcinoma or Papillary Urothelial Neoplasm of Low Malignant Potential? Urology. 86(2): 379-383. [PubMed.]
- Park S, Kim KS, Cho SJ, Lee DG, Jeong BC, et al. (2014) Urothelial Tumors of the Urinary Bladder in Two Adolescent Patients: Emphasis on Follow-up Methods. Korean J Urol. 55(6): 430-433. [PubMed.]