>Corresponding Author : Mehdi Belhakim
>Article Type : Research Article
>Volume : 3 | Issue : 6
>Received Date : 25 Sep, 2023
>Accepted Date : 07 Oct, 2023
>Published Date : 12 Oct, 2023
>DOI : https://doi.org/10.54289/JCRMH2300130
>Citation : Belhakim M, Chawki K, Ettagmouti Y and Habbal R. (2023) Tuberculous Pericarditis: Clinical, Diagnostic, and Therapeutic Features. J Case Rep Med Hist 3(6): doi https://doi.org/10.54289/JCRMH2300130
>Copyright : © 2023 Belhakim M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Research Article | Open Access | Full Text
1University Hospital Center Ibn Rochd, Hospital Street, 20360 Casablanca, Morocco
2Cardiology department, University Hospital Ibn Rochd, University Hassan II, Casablanca, Morocco
*Corresponding author: Mehdi Belhakim, Cardiology department, University Hospital Ibn Rochd, University Hassan II, Casablanca, Morocco
Abstract
Introduction: Tuberculous pericarditis is a rare manifestation of extrapulmonary tuberculosis. Due to the infrequency of this condition, the most effective management approach has not been clearly established. Our study analyzed 14 cases with tuberculous pericarditis treated at Ibn Rochd Hospital in Casablanca over two years from 2020 to 2022.
Methods: Medical records of tuberculous pericarditis patients were reviewed. Data on demographics, clinical presentation, diagnostic methods, and treatments were collected. Results were expressed in terms of frequencies, averages, and percentages.
Results: The mean patient age was 37.7 years, with 64% males. Common symptoms included fever (50%), chest pain (57%), and dyspnea (92.8%). Clinical signs included right heart failure (35%) and muffled heart sounds (57%). ECG findings showed sinus tachycardia (71.4%) and low voltage (57%).
Echocardiography revealed pericardial effusion (78%) and other abnormalities.
Pericardial fluid was mostly citrine yellow (64%) and serohemorrhagic (36%). Adenosine deaminase was positive in 57% of cases. GeneXpert confirmed 71% of cases, while pericardial biopsy confirmed 29%. All received antitubercular treatment, with corticosteroids in three cases. In-hospital, 92% showed pericardial effusion regression, but one death due to tamponade occurred. Long term, 21% had effusion recurrence, and 35% transitioned to constrictive pericarditis.
Conclusion: Tuberculous pericarditis presents diagnostic challenges. Clinical, radiological, and biological evidence is crucial for diagnosis. Antitubercular treatment is effective, but the risk of constrictive pericarditis remains high, necessitating further research into corticosteroid therapy's role in prevention.
Keywords: Pericarditis; Extrapulmonary Tuberculosis; Diagnostic; Therapeutic; Cardiology; Morocco
Abbreviations: EPTB: Extrapulmonary Tuberculosis, TB: Tuberculosis, CHU: University Hospital Center, ECG: Electrocardiogram, ADA: Adenosine Deaminase, PCR: Polymerase Chain Reaction
Introduction
Extrapulmonary tuberculosis (EPTB) is on the rise, accounting for an increasing percentage of all tuberculosis (TB) cases, typically ranging from 20% to 40% in various studies [1]. Among the diverse manifestations of EPTB, tuberculous pericarditis stands out as a rare occurrence, being identified in approximately 1% of all autopsied TB cases and in 1% to 2% of pulmonary TB cases [2]. Given the scarcity of this condition, establishing an optimal management approach has remained a challenge [3]. Consequently, our study aims to provide an in-depth description of the clinical, diagnostic, and therapeutic attributes observed in 14 patients diagnosed with tuberculous pericarditis.
Materials and Methods
Study Design, Location, and Duration
This study is a retrospective, descriptive, and single-center investigation conducted in the Internal Medicine Department of the University Hospital Center (CHU) in Casablanca. The study involved the retrieval and analysis of medical records pertaining to patients diagnosed with tuberculous pericarditis. The study period encompassed a span of 2 years, from January 2020 to December 2022.
Study Population
Inclusion Criteria: This study included patients under the care of the Cardiology Department in Casablanca diagnosed with tuberculous pericarditis based on a combination of clinical, biological, and echocardiographic criteria.
Exclusion Criteria: Patients whose diagnosis of tuberculous pericarditis did not meet international diagnostic criteria and those in whom pericardial effusion was not directly attributed to tuberculosis were excluded from the analysis.
Data Collection
Data were extracted from the medical records of patients admitted to the Cardiology Department during the specified timeframe using a structured data collection grid. The collected data encompassed the following categories:
• Sociodemographic information (age, gender, and place of origin).
• Medical history (including comorbidities such as diabetes, hypertension, heart diseases, lung diseases, and a history of exposure to toxins or specific medications, as well as family history of similar conditions).
• Presentation details of tuberculosis (circumstances of diagnosis, date of symptom onset, and mode of symptom presentation).
• Clinical manifestations (including dyspnea, fatigue, and chest pain).
• Physical examination findings.
• Electrocardiogram (ECG) and cardiac Doppler echocardiography findings.
• Laboratory test results.
• Details of various therapeutic protocols administered.
• Follow-up duration.
• Types and rates of complications encountered during the course of treatment.
Results
Among the 14 patients included, the mean age was 37.7 years, ranging from 22 to 67 years. A male predominance was observed, with 64% of patients being male. The most frequently reported clinical symptoms were fever (50%), chest pain (57%), and dyspnea (92.8%), mainly categorized as NYHA Class III. Clinical examination revealed signs of right heart failure in 35% of cases, muffled heart sounds (57%), arterial hypotension (14.2%), and tachycardia (71.4%). ECG showed sinus tachycardia in 71.4% of cases, low voltage (57%), and electrical alternans in 14.2% (figure 1).
Transthoracic echocardiography revealed significant pericardial effusion in 78% of cases (figure 2), significant mitral or tricuspid flow variation in 28.5%, compression of right heart chambers in 14.2%, and inferior vena cava dilation in 64% of cases.
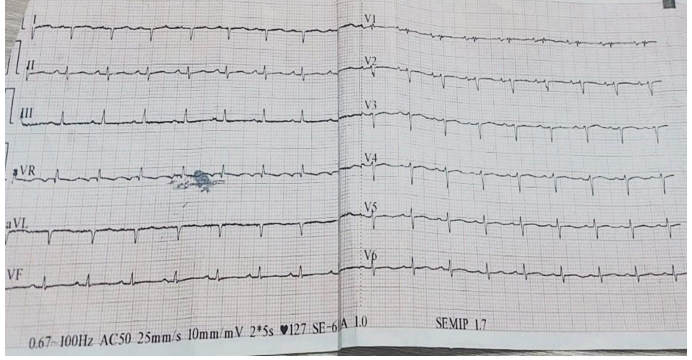
Figure 1: Sinus tachycardia with a low voltage on EKG
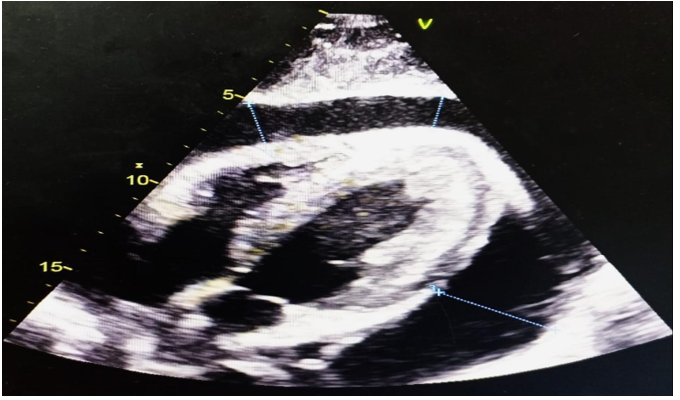
Figure 2: Pericardial Effusion with Secondary Right Ventricular Compression due to Tuberculous Pericarditis
The fluid appeared citrine yellow in 64% of cases and serohemorrhagic in 36% of patients, with an exudative predominance and lymphocytic predominance in 71%. Adenosine deaminase (ADA) levels were positive in 57% with a median value of 56 IU/L. The diagnosis was confirmed via GeneXpert in association with a clinical, radiological, and biological argument in 71% of cases and by pericardial biopsy in 29% of cases. All patients received antitubercular treatment. Corticosteroid therapy was used in 3 patients. In-hospital progression was favorable, with pericardial effusion regression in 92% of patients. One case of death occurred due to tamponade. Long-term evolution showed pericardial effusion recurrence in 21% of patients and transition to constrictive pericarditis in 35% of cases.
Discussion
The primary clinical manifestations of tuberculous pericarditis manifest as profound dyspnea, concomitant with a triad of persistent cough and thoracic discomfort. Concurrent clinical presentations often encompass orthopnea, progressive reduction in body mass, and peripheral edema localized to the ankles. Regarding clinical markers, frequently observed findings include the presence of a discernible pericardial friction rub, an elevated body temperature, and an elevated heart rate. Noteworthy supplementary observations may encompass pulsus paradoxus, hepatomegaly, engorged jugular veins, the manifestation of pleural effusion, and the identification of attenuated cardiac auscultations [4,5]. Our patients exhibited nearly all of these indications. Echocardiography stands as a precise and non-invasive modality for the diagnosis of pericardial effusion [6]. Echocardiographic results demonstrating effusion with fibrinous strands adhering to the visceral pericardium are characteristic, albeit not exclusively diagnostic, for a tuberculous etiology [7]. Complementary insights can be gleaned through imaging modalities such as CT scanning or MRI, which provide incremental data to augment echocardiography [8,9]. Surface myocardial inflammation is believed to elucidate the four stages of ECG changes that become evident during acute pericarditis. These stages encompass widespread, upwardly concave ST-segment elevation, T-wave inversion, and PR-segment depression. The progression of these electrocardiographic changes aids in distinguishing pericarditis from early repolarization and acute myocardial infarction [10]. The presence of microvoltage suggests a substantial pericardial effusion, and cardiac tamponade is improbable when ECG microvoltage is absent. In cases where tuberculosis is suspected, pericardiocentesis is advised [11]. In more than 80% of instances of tuberculous pericarditis, the pericardial fluid exhibits a sanguineous quality. Therefore, confirming tuberculosis as the underlying cause remains imperative, as malignancies and delayed sequelae of penetrating trauma may also yield bloody pericardial effusions. Tuberculous pericardial effusion typically presents as an exudate characterized by elevated protein content and an increased leukocyte count, with a predominance of lymphocytes and monocytes [2]. The tuberculous origin of pericarditis should ideally be ascertained through the detection of M. tuberculosis infection evidence, including acid-fast bacilli and pericardial fluid culture, or via histological examination of pericardial tissue. In cases where pericardial fluid cannot be safely obtained percutaneously, pericardial biopsy serves as an alternative method to establish a definitive diagnosis of tuberculous pericarditis. Tissue histology is preferable as an initial diagnostic approach [12,13]. Polymerase chain reaction (PCR) has also been suggested as a direct means of detecting M. tuberculosis DNA or RNA in pericardial fluid [14]. Due to the elevated mortality risk associated with untreated tuberculous pericarditis and the prolonged culture periods required for conventional tests, therapeutic decisions are frequently rendered before direct diagnostic results become available. Tuon's studies have demonstrated that an elevated pericardial ADA activity suggests tuberculous pericarditis. A pericardial ADA level ≥40 U/L exhibits a sensitivity and specificity of 88% and 83%, respectively [15]. Treatment often needs to be initiated based on indirect test outcomes before a bacteriological diagnosis is confirmed. A regimen comprising rifampicin, isoniazid, pyrazinamide, and ethambutol for a minimum of 2 months, followed by isoniazid and rifampicin (totaling 6 months of therapy), has shown high efficacy in treating patients with extrapulmonary tuberculosis. Extending treatment beyond 9 months does not yield superior outcomes and is encumbered by increased costs and poor adherence [16]. Constrictive pericarditis ensues in approximately 18% to 46% of patients with tuberculous pericardial effusion, even with antituberculosis medication and corticosteroid treatment. The management of tuberculous pericardial constriction entails administering standard antituberculosis drugs for 6 months, alongside pericardiectomy if clinical evidence of constriction persists despite drug therapy [17,18]. Managing effusive-constrictive pericarditis presents challenges since pericardiocentesis fails to alleviate impaired cardiac filling, and surgical removal of fibrinous exudate adhering to the visceral pericardium is unfeasible. Antituberculosis drugs should be administered, and serial echocardiography should be performed to identify pericardial adhesions amenable to surgical stripping. The role of corticosteroids in such patients remains uncertain [4]. Our study has enabled us to evaluate the diagnostic and therapeutic approaches to Moroccan patients with tuberculous pericarditis over the past 2 years within our hospital setting. This evaluation has elucidated the limitations inherent in the current methodology and has provided insights into the evolving profiles of these patients. This, in turn, can serve as a foundation for the development of an enhanced strategy for screening, diagnosis, and treatment through interdisciplinary collaboration between infectious disease specialists and cardiologists, with the aim of substantially improving patient prognoses. Nevertheless, akin to other investigations, our work has its constraints. The limited patient cohort [14] does not constitute a statistically robust sample size to infer significant results. Additionally, the retrospective nature of our study represents a substantial limitation. Lastly, data retrieval was reliant on non-computerized medical records, at times lacking comprehensive follow-up and patient progression details. This underscores the necessity for implementing a computerized platform to facilitate more comprehensive data collection.
Conclusion
Tuberculous pericarditis poses diagnostic complexities, relying on a triad of clinical, radiological, and biological markers for accurate identification. While antitubercular treatment demonstrates efficacy, the persistent risk of constrictive pericarditis underscores the need for continued investigation into the potential preventative role of corticosteroid therapy.
Declarations
Consent for publication: Written informed consent was obtained from the patients for publication of this case report and any accompanying images.
Availability of data and material: All data analysed during this study are included in this published article.
Competing interests: The authors declare that they have no competing interests.
Author contributions:
Mehdi Belhakim: writing paper
Khawla Chawki: study concept literature
Yassine Ettagmouti: interpretation and analysis
Rachida Habbal: Interpretation and analysis
References
- Mazza-Stalder J, Nicod L, Janssens JP. (2012) La tuberculose extrapulmonaire. Revue des maladies respiratoires. 29(4): 566-578. [Ref.]
- Mayosi BM, Burgess LJ, Doubell AF. (2005) Tuberculous pericarditis. Circulation. 112(23): 3608‑3616. [Ref.]
- Trautner BW, Darouiche RO. (2001) Tuberculous pericarditis: optimal diagnosis and management. Clinical infectious diseases. 33(7): 954‑961. [PubMed.]
- Fowler NO. (1991) Tuberculous pericarditis. Jama. 266(1): 99‑103. [PubMed.]
- Reuter H, Burgess L, Van Vuuren W al, Doubell A. (2006) Diagnosing tuberculous pericarditis. Journal of the Association of Physicians. 99(12): 827‑839. [Ref.]
- George S, Salama AL, Uthaman B al, Cherian G. (2004) Echocardiography in differentiating tuberculous from chronic idiopathic pericardial effusion. Heart. 90(11): 1338‑1339. [Ref.]
- Liu PY, Li YH, Tsai WC, Tsai LM, Chao TH, et al. (2001) Usefulness of echocardiographic intrapericardial abnormalities in the diagnosis of tuberculous pericardial effusion. American Journal of Cardiology. 87(9): 1133‑1135. [PubMed.]
- Gulati GS, Sharma S. (2004) Pericardial abscess occurring after tuberculous pericarditis: image morphology on computed tomography and magnetic resonance imaging. Clinical radiology. 59(6): 514‑519. [PubMed.]
- Khera G, Chowdhury V, Singh S, Dixit R. (2005) Magnetic resonance imaging of effusive constrictive pericarditis. Indian heart j. 57(6): 780-782. [PubMed.]
- Ariyarajah V, Spodick DH. (2007) Acute pericarditis: diagnostic cues and common electrocardiographic manifestations. Cardiology in review. 15(1): 24‑30. [PubMed.]
- Little WC, Freeman GL. (2006) Pericardial disease. Circulation. 113(12): 1622‑1632. [PubMed.]
- Cherian G. (2004) Diagnosis of tuberculous aetiology in pericardial effusions. Postgraduate medical journal. 80(943): 262‑266. [Ref.]
- Corey GR, Campbell PT, Van Trigt P, Kenney RT, O’Connor CM, et al. (1993) Etiology of large pericardial effusions. The American journal of medicine. 95(2): 209‑213. [PubMed.]
- Lee JH, Lee CW, Lee SG, Yang HS, Hong MK, et al. (2002) Comparison of polymerase chain reaction with adenosine deaminase activity in pericardial fluid for the diagnosis of tuberculous pericarditis. The American journal of medicine. 113(6): 519‑521. [PubMed.]
- Tuon FF, Litvoc MN, Lopes MIBF. (2006) Adenosine deaminase and tuberculous pericarditis-a systematic review with meta-analysis. Acta tropica. 99(1): 67‑74. [PubMed.]
- Maisch B. (2003) Practical aspects of the management of pericardial disease. Heart. 89(9): 1096‑1103. [Ref.]
- Desai HN. (1979) Tuberculous pericarditis-a review of 100 cases. South African Medical Journal. 55(22): 877‑880. [PubMed.]
- Sagrista-Sauleda J, Permanyer-Miralda G, Soler-Soler J. (1988) Tuberculous pericarditis: ten year experience with a prospective protocol for diagnosis and treatment. Journal of the American College of Cardiology. 11(4): 724‑728. [PubMed.]