>Corresponding Author : Yassine Ettagmouti
>Article Type : Case Report
>Volume : 3 | Issue : 4
>Received Date : 30 March, 2023
>Accepted Date : 20 April, 2023
>Published Date : 20 May, 2023
>DOI : https://doi.org/10.54289/JCRMH2300117
>Citation : Ettagmouti Y, Belhakim M, Bennani G and Habbal R. (2023) Heyde Syndrome, A Rare Cause of Digestive Bleeding: About a Case Report and Literature Review. J Case Rep Med Hist 3(4): doi https://doi.org/10.54289/JCRMH2300117
>Copyright : © 2023 Ettagmouti Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
Cardiology Department, Ibn Rochd hospital university, Casablanca, Morocco
*Corresponding author: Yassine Ettagmouti, Cardiology Department, Ibn Rochd hospital university, Casablanca, Morocco
Abstract
Heyde's syndrome is a rare condition that usually affects the elderly population and is responsible for a high mortality rate due to delayed diagnosis.
It is characterized by the triad of aortic stenosis (AS), gastrointestinal bleeding due to angiodysplastic lesions and acquired Willebrand factor deficiency,
We report the case of a 68-year-old patient who consulted the emergency department for an anemic syndrome secondary to low GI bleeding with severe aortic stenosis on echocardiography.
The patient underwent an emergency transfusion of packed red blood cells with a colonoscopy confirming a colonic angiodysplasia lesion. The decision was an aortic valve replacement with a good subsequent evolution.
Aortic valve replacement reduces gastrointestinal bleeding in the majority of patients with angiodysplasia, whereas gastrointestinal surgery results in remission only in rare patients.
Key words: Heyde Syndrome, Aortic Valve Replacement, Case Report
Abbreviations: AS: Aortic Stenosis; TAVI: Transcatheter Aortic Valve Implantation
Introduction
In 1958, Edward Heyde first described a multisystem disorder characterised by the triad of aortic stenosis (AS), gastrointestinal bleeding due to angiodysplasia lesions and acquired Willebrand factor deficiency, known as Heyde syndrome [1]. This is a rare and serious disease that usually affects the elderly and is responsible for a high mortality rate, especially in the absence of early diagnosis and adequate management [2]. Indeed, aortic valve replacement significantly reduces the risk of GI bleeding in most patients [3]. Thus, clinicians should be aware of Heyde's syndrome to ensure prompt diagnosis and appropriate management.
We report a case of an elderly patient of 68 years who consult for an anemic syndrome secondary to rectal bleeding with a severe aortic stenosis on echocardiography who received an aortic valve replacement with good outcome.
Case presentation
We report the case of a 68-year-old man, known to be hypertensive on a 5mg/day converting enzyme inhibitor, treated for pleural tuberculosis 30 years ago without recurrence of tuberculosis, smoking cessation 20 years ago.
There was no notion of recent medication or plants.
The patient consulted the emergency room for exertional dyspnea worsening for 1 month, associated with three episodes of low-level externalized digestive bleeding trivialized by the patient.
Physical examination revealed a conscious patient with a blood pressure of 115/60 mmHg, polypneic at 32 breaths/min, oxygen saturation of 96%, heart rate of 115 bpm, apyretic with mucocutaneous pallor. The cardiovascular examination noted an ejection murmur at the aortic focus, the pleuropulmonary examination was unremarkable.
The rectal examination came back soiled with blood.
Electrocardiogram revealed sinus tachycardia with left ventricular hypertrophy with secondary repolarization disorders.
Complete blood count showed microcytic hypochromic anemia (hemoglobin 7.5 gr/dl), white blood cell count 8830/mm3, platelets 203,000/mm3, hemostasis was normal, glomerular filtration rate 67ml/min/m².
A request for packed red blood cells was made urgently, with spread transfusion of 2 packed red blood cells with a control hemoglobin of 10.1 gr/dl, antihypertensive treatment was maintained.
The echocardiography showed very severe aortic stenosis (aortic area:0.6 cm² by planimetry, 0.5cm² by continuity equation, mean gradient at 89mmHg, Vmax at 5.75m/s, Permeability index at 19% with thickened and calcified aortic sigmoid (Figure 1).
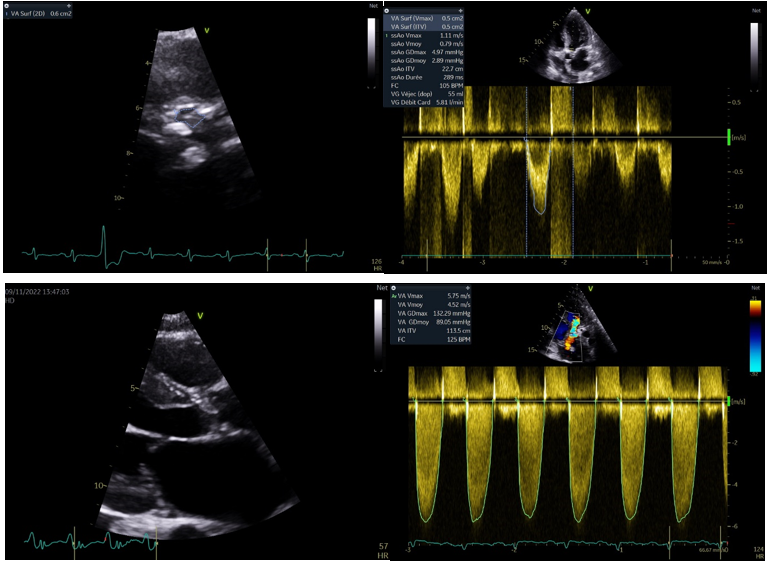
Figure 1: Echocardiographic parameters of very severe aortic stenosis
In addition, the left ventricular ejection fraction was 62% in Simpson biplane, minimal concentric left ventricular hypertrophy, no other associated valvulopathies, good right ventricular function and no pericardial effusion.
An oesogastroduodenal fibroscopy was normal, colonoscopy under sedation was performed, showing a colonic angiodysplasia lesion (Figure 2).

Figure 2: Colonoscopy showing colonic angiodysplasia
In view of the anemia, the intestinal angiodysplasia and the aortic narrowing we concluded to a syndrome of heyde
The patient underwent aortic valve replacement under extracorporeal circulation with a good postoperative evolution.
Regression of the aortic narrowing was noted with a normal aortic surface at the control echocardiography after 3 months postoperatively.
Discussion
Since the first case described by HEYDE in 1958, several studies published a few years later have discussed the pathophysiological basis of HEYDE syndrome, the main predisposing factor for bleeding in this population is acquired Willebrand factor deficiency resulting from the haemodynamic stress induced by the calcified aortic valve [2,4-6].
This syndrome is typically a disease of the elderly population, most often diagnosed in patients over 65 years of age. Indeed, the prevalence of aortic stenosis is 7.5% in patients aged 75 years or older [7]. The rate of clinically significant gastrointestinal bleeding related to angiodysplasia lesions is estimated to be 1-3% in patients with moderate to severe AS [8].
Clinicians should carefully assess the cardiovascular, digestive and haematological systems for clinical signs of AS (dyspnoea, chest pain, syncope, systolic murmur at the aortic site...), external or occult bleeding or haemostasis disorders. The initial biological work-up should include a blood count, metabolic work-up, haemostasis work-up and a stool blood test. An electrocardiogram for electrical signs of AS and a cardiac Doppler ultrasound should also be performed to assess the valve disease and its impact on the heart. Other endoscopic and imaging tests may be performed depending on the initial assessment [9].
Aortic valve replacement reduces gastrointestinal bleeding in 93% of patients with angiodysplasia, whereas gastrointestinal surgery results in remission in only 5% of patients [10]. Benton and colleagues demonstrated that transcatheter aortic valve implantation (TAVI) stops massive bleeding in a patient with Heyde syndrome [11]. Indeed, TAVI is preferred to surgical aortic valve replacement because it is a safer modality with lower postoperative risk [12]. Due to the high bleeding risk in patients with mechanical prosthesis receiving wafarin, bioprostheses should be preferred.
Conclusion
Heyde's syndrome is a complex, multisystem disorder that requires adequate management to prevent life-threatening bleeding complications. Aortic valve replacement significantly reduces GI bleeding and improves the prognosis of these patients. This syndrome is still not well known, hence the need for greater awareness among practitioners.
Declarations
Consent for publication: Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Ethical approval: As international standard, written ethical approval has been collected and preserved by the authors.
Availability of data and material: All data generated or analysed during this study are included in this published article.
Competing interests: The authors declare that they have no competing interests.
References
- Heyde EC. (1958) Gastrointestinal bleeding in aortic stenosis. N Engl J Med. 259: 196. [PubMed.]
- Rosa VEE, Ribeiro HB, Fernandes JRC, Santis A de, Spina GS, et al. (2021) Heyde’s Syndrome: Therapeutic Strategies and Long-Term Follow-Up. Arquivos Brasileiros de Cardiologia. 117: 512‑517. [PubMed.]
- Thompson JL, Schaff HV, Dearani JA, Park SJ, Sundt TM, et al. (2012) Risk of recurrent gastrointestinal bleeding after aortic valve replacement in patients with Heyde syndrome. The Journal of Thoracic and Cardiovascular Surgery. Juill. 144(1): 112‑116. [PubMed.]
- Warkentin TE, Moore JC, Anand SS, Lonn EM, Morgan DG. (2003) Gastrointestinal bleeding, angiodysplasia, cardiovascular disease, and acquired von Willebrand syndrome. Transfusion medicine reviews. 17(4): 272‑286. [Ref.]
- Morishima A, Marui A, Shimamoto T, Saji Y, Tambara K, et al. (2007) Successful aortic valve replacement for Heyde syndrome with confirmed hematologic recovery. The Annals of thoracic surgery. 83(1): 287‑288. [Ref.]
- Loscalzo J. (2012) From clinical observation to mechanism-Heyde’s syndrome. New England Journal of Medicine. 367(20): 1954‑1956. [PubMed.]
- Blackshear JL. (2019) Heyde syndrome: aortic stenosis and beyond. Clinics in geriatric medicine. 35(3): 369‑379. [PubMed.]
- Undas A, Natorska J. (2015) Bleeding in Patients with Severe Aortic Stenosis in the Era of Transcatheter Aortic Valve Replacement. JACC: Cardiovascular Interventions. Avr. 8(5): 701‑703. [PubMed.]
- Theis SR, Turner SD. (2021) Heyde syndrome. In: StatPearls [Internet]. StatPearls Publishing. [Ref.]
- Pate GE, Chandavimol M, Naiman SC, Webb JG. (2004) Heyde’s syndrome: a review. Journal of Heart Valve Disease. 13(5): 701‑712. [PubMed.]
- Benton Jr SM, Kumar A, Crenshaw M, Fredi JL. (2014) Effect of transcutaneous aortic valve implantation on the Heyde’s syndrome. The American Journal of Cardiology. 114(6): 953‑954. [Ref.]
- Muntaner C, Nagoshi C, Jaffe JH, Walter D, Haertzen C, et al. (1989) Correlates of self-reported early childhood aggression in subjects volunteering for drug studies. The American journal of drug and alcohol abuse. 15(4): 383‑402. [PubMed.]