>Corresponding Author : Yassine Ettagmouti
>Article Type : Case Report
>Volume : 2 | Issue : 7
>Received Date : 02 Nov, 2022
>Accepted Date : 14 Nov, 2022
>Published Date : 21 Nov, 2022
>DOI : https://doi.org/10.54289/JCRMH2200132
>Citation : Ettagmouti Y, Maaroufi A, Rochd M and Habbal R. (2022) Carbamazepine Induced Myocarditis in an Epileptic Adolescent: A Rare Case Report. J Case Rep Med Hist 2(7): doi https://doi.org/10.54289/JCRMH2200132
>Copyright : © 2022 Ettagmouti Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
Ibn Rochd Hospital University, Casablanca, Morocco
*Corresponding author: Yassine Ettagmouti, Ibn Rochd Hospital University, Casablanca, Morocco
Abstract
Myocarditis is an inflammation of the heart muscle with on histological examination an infiltrate of inflammatory cells and signs of myocyte necrosis.
Our case illustrates a toxic myocarditis secondary to the intake of carbamazepine with a good improvement during the evolution which makes the case rare.
We report a case of 16 years old female, recently diagnosed with epilepsy treated with carbamazepine admitted to the cardiology department for chest pain and shortness of breath. On admission, the patient was haemodynamically stable.
The dosage of ultrasensitive troponins was very high on admission, indicating myocyte necrosis that could probably be related to myocarditis confirmed by cardiac MRI.
After diagnostic confirmation, an etiological assessment was performed, revealing a skin eruption with the presence of multiple adenopathies and hypereosinophilia on the biological assessment falling within the framework of a DRESS syndrome (drug reaction with eosinophilia and systemic symptoms) in connection with the taking of carbamazepine. The evolution of the patient was good with regression of the symptoms under medical treatment and clinical echocardiographic monitoring.
Keep in mind that myocarditis can mimic an acute coronary syndrome and that MRI has become an essential diagnostic tool for confirmatory diagnosis. The etiology of the myocarditis will be sought in a second step, essential for the specific treatment according to the incriminated cause. It is always necessary to look for a notion of drug intake which can be incriminated as a cause of myocarditis.
Keywords: Case Report; Carbamazepine; Myocarditis; DRESS Syndrome
Abbreviations: DRESS: Drug Reaction with Eosinophilia and Systemic Symptoms
Introduction
Myocarditis is an inflammation of the heart muscle with on histological examination an infiltrate of inflammatory cells and signs of myocyte necrosis [1].
DRESS syndrome (drug reaction with eosinophilia and systemic symptoms) is a febrile rash associated with systemic manifestations that can develop in both paediatric and adult patients [2].
In this report, we describe the case of an epileptic 16-year-old female with a myocarditis induced by carbamazepine with a good evolution on the follow-up which is a rare situation.
Cases presentation
We report a case of 16 years old female, recently diagnosed with epilepsy treated with carbamazepine 400mg once a day for a duration of 4 weeks.
There was no current or past use of cocaine or other drugs, no history of recent chest wall trauma, no notion of recent viral infection and she had no familial history of cardiac disease.
She presented at the emergency department of our institution with intense substernal chest pain and shortness of breath. She perceived some relief of pain with anteflexed position change and exacerbation upon inspiration.
In the patient’s physical examination, a temperature of 38.2°C, heart rate of 105 beats/minute, respiratory rate of 22 breaths/minute, blood pressure of 115/60 mmHg, and O2 saturation of 96% were measured. Cardio Pulmunary auscultation revealed a well perceived S1 S2 with no rales or crackles on lungs sounds and no signs of right heart failure. It was notable the presence of diffuse macular rash and palpable centimetric axillary and cervical lymph nodes.
The initial EKG revealed sinus rhythm with ST elevation in inferior leads with ST depression in antero septal territory (Figure1).
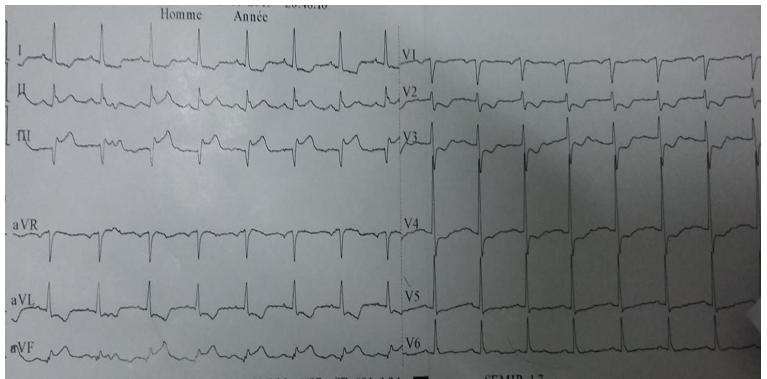
Figure 1: ST depression in antero septal territory
Results of initial cardiac enzyme tests revealed a troponin HS of 18 200ng/L.
Laboratory findings revealed also: haemoglobin 14.7 gr/dl, leucocytes 8880/mm3, 47% neutrophil, 40% lymphocytes, 3% monocytes, 10% eosinophil, total eosinophil count 888/mm3, thrombocytes 214 000/mm3 AST 32 IU/l, CRP 45 mg/dl, VS = 30mm.
Serological studies of syphilis, HSV, cytomegalovirus, Epstein-Barr virus, hepatitis A, B, and C, HIV, and adenovirus were normal.
A chest radiograph clear lungs with a normal-sized cardiac silhouette.
We performed pcr and serology IgM and Ig G of coronavirus with negative results
Echocardiography showed normal wall motion, with an ejection fraction of 64%, no significant heart valvular disease and no pericardial effusion.
There was a normal longitudinal strain rate of -20.9% (Figure 2).
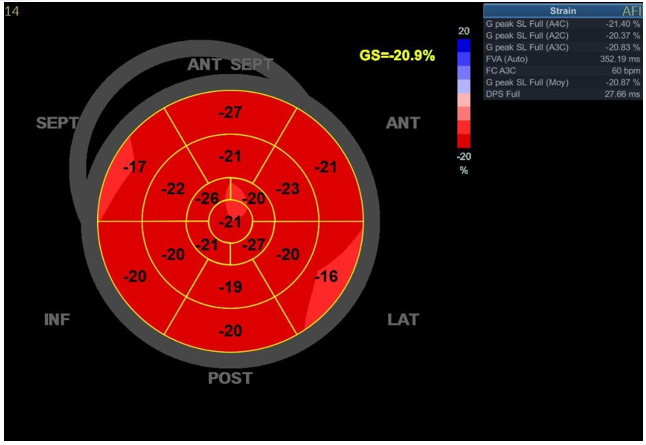
Figure 2: Bull's eye, VG strain
A cardiac MRI was performed, showing enhanced signal intensity in T2weighted sequences, interesting lateral basal, which translate subepicardial edema.
Perfusion sequences displayed no late Gadolinium Enhancement in the same segments described above with respect of endocardium (Figure 3).
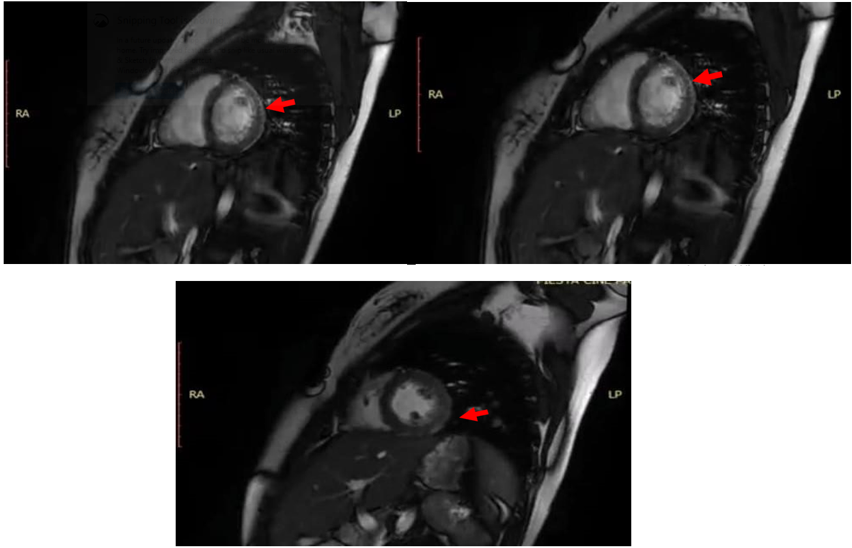
Figure 3: Cardiac MRI sequences
Cine imaging analysis showed normal LV systolic function without cavitary dilatation LVEF = 60%.
These findings concluded to a subacute myocarditis.
Overall, our patient had a hypersensitivity reaction to carbamazepine with Fever, rash, and eosinophilia occurring weeks after the start of carbamazepine therapy complicated with myocarditis with lead to change of his antiepileptic therapy by neurologist to levetiracem 250mg twice daily with good tolerance and introduction of oral corticosteroid therapy for 8 weeks.
During follow up it was noted the regression of rash, resolution of chest pain and dyspnea.
Discussion
Myocarditis is by an inflammatory myocardial disease defined on validated histological and immunological criteria, associated with myocardial necrosis of non-ischemic origin [1].
MRI has avoided invasive diagnostic procedures and has facilitated the diagnosis of myocarditis can present in a multitude of clinical presentations ranging from simple dyspnea or chest pain to cardiogenic shock or sudden death [3].
Infectious causes, in particular viral causes, are the most implicated in acute myocarditis. To this are added the hypersensitivity reactions, systemic and autoimmune diseases.
Eosinophilic myocarditis can be a potentially life-threatening complication of a drug reaction with systemic symptoms being part of the DRESS syndrome [4].
DRESS syndrome is a febrile rash associated with systemic manifestations that can develop in both paediatric and adult patients.
The aetiology of DRESS syndrome is not fully understood, many drugs are blamed, at their head aromatic anticonvulsants [2,5].
Yang et al. reported that carbamazepine and phenytoin, which are anticonvulsant medications, were responsible for 43.6% of all DRESS syndrome cases
Diagnostic criteria defined by the RegiSCAR study group and the Japanese consensus group are used for the diagnosis of DRESS syndrome. In addition, diagnostic criteria are also defined by Bocquet et al.
To meet the DRESS definition, patients must have three of the four main RegiSCAR criteria in the table below [5].
The RegiSCAR scoring system grades DRESS cases as "no," "possible," "probable," or "definite".
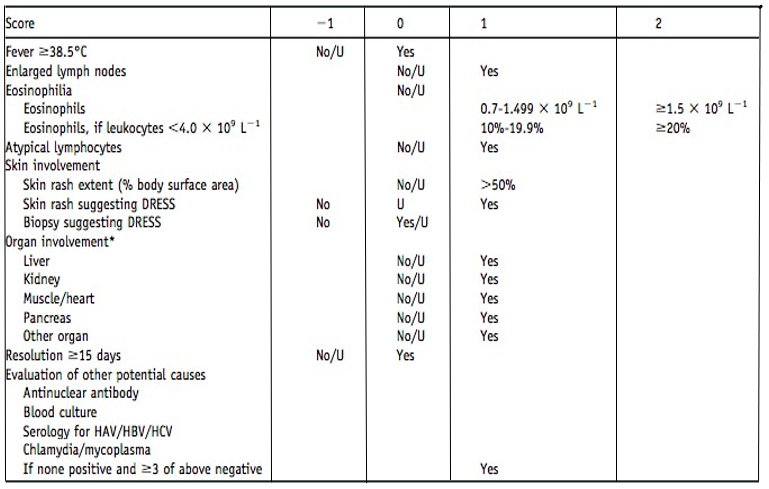
The Japanese consensus group developed a second diagnostic criterion group. According to these criteria, seven of the criteria or all of the first five criteria must be present for the diagnosis.
There is no consensus on the treatment of myocarditis. Hospitalization is recommended in a unit intensive care with cardiac monitoring, because the evolution is unpredictable.
Treatment of eosinophilic myocarditis includes stopping the causative drug and corticosteroids [6]. The use of positive inotropic drugs may be necessary in case of cardiogenic shock
In the literature, there are only a few cases of myocarditis secondary to the use of anti-epileptic drugs. These cases usually progress to death and are diagnosed during autopsy.
Our case illustrates a good evolution of acute myocarditis secondary to carbamazepine intake in a 16-year-old girl and is one of the rare cases found on the previous reported cases.
Conclusion
Lessons to be learned from this case report are that:
Acute myocarditis can be a life-threatening situation which requires early diagnosis and treatment.
Do not forget to look for medication that can cause myocarditis.
Carbamazepine is one of the treatments implicated in the occurrence of myocarditis.
Declarations
Consent for publication: Written informed consent was obtained from the patients for publication of this case report and any accompanying images.
Availability of data and material: All data generated or analysed during this study are included in this published article.
Competing interests: The authors declare that they have no competing interests.
Author contributions
Ettagmouti Y: writing paper
Maaroufi A: study concept literature
Rochd M: care of the patient
Habbal R: Interpretation and analysis
References
- Vos T, et al. (2015) Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: A systematic analysis for the Global Burden of Disease Study. Lancet 2013. 386: 743-800. [PubMed.]
- Sullivan JR, Shear NH. (2001) The drug hypersensitivity syndrome: What is the pathogenesis? Arch Dermatol. 137: 357-364. [PubMed.]
- Lindsay J, Pichard AD. (1984) Acute myocardial infarction with normal coronary arteries. Am J Cardiol. 54: 902-904. [PubMed.]
- Kano Y, Shiohara T. (2009) The variable clinical picture of drug-induced hypersensitivity syndrome/drug rash with eosinophilia and systemic symptoms in relation to the eliciting drug. Immunol Allergy Clin North Am. 29: 481-501. [PubMed.]
- Kardaun SH, Sidoroff A, Valeyrie-Allanore L, et al. (2007) Variability in the clinical pattern of cutaneous side-effects of drugs with systemic symptoms: does a DRESS syndrome really exist? Br J Dermatol. 156: 609-611. [PubMed.]
- Lin YC, Oliveira GH, Villa-Forte A. (2013) Churg-Strauss syndrome and persistent heart failure: active disease or damage? J Clin Rheumatol. 19: 390-392. [PubMed.]