>Corresponding Author : Ishan Sardesai
>Article Type : Case Report
>Volume : 2 | Issue : 2
>Received Date : 27 June, 2022
>Accepted Date : 10 July, 2022
>Published Date : 14 July, 2022
>DOI : https://doi.org/10.54289/JCRMH2200110
>Citation : Sardesai I, Pillai S, Bishnoi AK and Shetty S. (2022) Management of Tracheal Stent Granulations: A Novel Approach. J Case Rep Med Hist 2(2): doi https://doi.org/10.54289/JCRMH2200110
>Copyright : © 2022 Sardesai I, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Junior Resident, Department of ENT, Kasturba Hospital, Manipal
2Professor and Unit Head, Department of ENT, Kasturba Hospital, Manipal
3Professor, Department of Cardiothoracic Surgery, Kasturba Hospital, Manipal
4Assistant Professor, Department of ENT, Kasturba Hospital, Manipal
*Corresponding author: Ishan Sardesai, Junior Resident, Department of ENT, Kasturba Hospital, Manipal
Summary
This is a case of a 29 year old female, diagnosed with adenoid cystic carcinoma of trachea who had previously undergone bronchoscopy, de-bulking of the tumour, stenting of trachea with a metallic stent followed by a course of chemo-radiotherapy. She then presented to our hospital with complaints of breathing difficulty. On rigid telescopy of larynx, a metallic stent was visualised below the level of the vocal cords with a mass lesion over it narrowing the airway. Contrast enhanced CT scan of neck and thorax showed a tracheal stent with soft tissue thickening at proximal and distal ends.
By using VV-ECMO, in this patient we were able to perform satisfactory airway evaluation, biopsy of mass at upper and lower end of tracheal stent using a rigid bronchoscope with Hopkins telescope and optical forceps and KTP laser assisted excision of granulation tissue with full endoscopic visualisation and without any complications.
Abbreviations: SARTI: Stent-Associated Respiratory Tract Infection, LMA: Laryngeal Mask Airway, VV-ECMO: Venovenous Extracorporeal Membrane Oxygenation
Background
Malignant airway obstruction is now a major indication for the use of metallic stents. In this patient population, metallic stents have proven to relieve symptoms, and reduce work of breathing as well as health care utilization. Airway stabilization with a stent may also allow time for palliative chemotherapy and radiation to take effect [1].
The most common complication of stenting is formation of granulation tissue [2].
Therefore, this case is important as it illustrates the complications which may occur as a consequence of the usage of metallic tracheal stents and also how these complications can be appropriately managed using novel techniques.
Case Presentation
A 29 year old female was diagnosed 2 years back with adenoid cystic carcinoma of trachea. For this she underwent bronchoscopy, de-bulking of the tumour, stenting of trachea with a metallic stent in a hospital abroad. For chemo-radio therapy, she came to India. Following this, she was asymptomatic until she developed progressively worsening breathing difficulty, cough with foul smelling expectoration, halitosis and frequent throat clearing since the past 8-9 months. 4 months back she came to our emergency triage with breathing difficulty and was prescribed steroids and nebulisation following which her symptoms improved. However due to persisting breathing difficulty which worsened on exertion, she presented to our out patient department.
On examination, she was found to have a mild biphasic stridor. She was not in respiratory distress but became breathless on walking. The laryngeal framework was normal and there was no tenderness or palpable swelling. Her voice was normal.
Investigations
A rigid telescopy of the larynx was performed which revealed bilateral, normal and mobile vocal cords and adequate glottic airway. The metallic stent was visualised below the level of the vocal cords with a mass lesion over it narrowing the airway of the tracheal lumen.
Subsequently she underwent a contrast enhanced CT scan of neck and thorax which showed
• a tracheal stent with proximal end at C6 vertebra and distal tip about 3.6 cm proximal to carina
• heterogenous soft tissue lesion with subtle enhancement in posterior aspect of trachea at D3 vertebral level with intra-tracheal extension causing luminal narrowing suspicious for malignancy
• soft tissue thickening with enhancement at proximal aspect of stent at C6 vertebral level around 1.7cm distal to true vocal cord causing tracheal narrowing with narrowest diameter of 6mm? granulation tissue/? malignancy
• sub-centimetric para-tracheal and pre-carinal lymph nodes
• varying sized nodules scattered in both lungs suggestive of metastasis
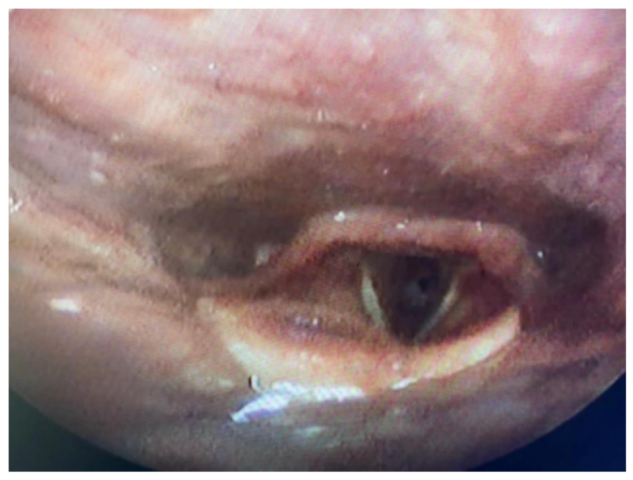
Image 1: Pre-operative rigid telescopy of larynx showing the narrowing of the tracheal airway
Treatment
This was a challenging situation as tracheostomy was not possible due to the presence of the metallic stent. Therefore, under veno-venous ECMO, she underwent airway evaluation, bronchoscopic biopsy of mass at upper and lower end of tracheal stent and KTP laser assisted excision of mass at upper end of tracheal stent. Following this, airway was noted to be improved.
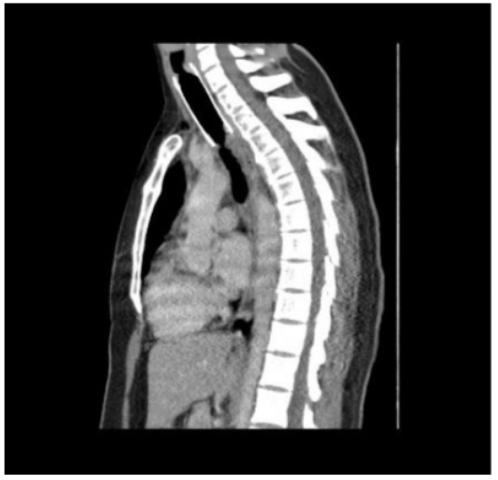
Image 2: Contrast enhanced CT scan of neck and thorax, sagittal section showing the tracheal stent
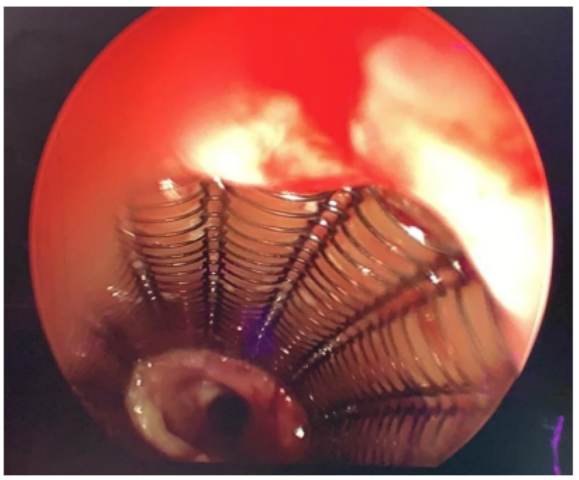
Image 3: Intra-operative image showing tracheal stent with granulation tissue at upper and lower end

Image 4: Veno-venous ECMO
She was monitored post operatively in cardio-thoracic ICU for a day and then shifted to the ENT ward. Her vitals were stable, there was no stridor and she had no complaints of breathing difficulty. She was discharged and advised to continue steroid inhaler for 1 week.
Outcome And Follow Up
On subsequent follow-up after one week, she was asymptomatic with no stridor or breathlessness on exertion.
The histopathology report was reported as granulation tissue from trachea with no evidence of malignancy.
The patient was reassured and advised to follow up every 6 months.

Image 5: Post operative rigid telescopy of larynx showing an improved tracheal airway
Discussion
Malignant airway obstruction is now a major indication for the use of metallic stents. In this patient population, metallic stents have proven to relieve symptoms, and reduce work of breathing as well as health care utilization. Although not curative, stents are effective means of palliating central airway obstruction and are often used in conjunction with other therapies to eradicate tissue. Airway stabilization with a stent may also allow time for palliative chemotherapy and radiation to take effect [1]. This was the approach followed in this patient when she was first diagnosed with adenoid cystic carcinoma of the trachea.
The most common complication of stenting is formation of granulation tissue which is more often seen when upper edge of stent is located at or below the vocal folds as was seen in this case [2]. Metallic stents as in this case, are more prone to develop granulations especially at the proximal segment, as they are more rigid with multiple edges and produce circumferential pressure on tissues, leading to airway irritation [3].
Another complication is stent-associated respiratory tract infection (SARTI) which probably involves 1 in 5 patients with airway stent [4]. Stent migrations, stent fractures, sputum retention, halitosis may also occur [5,6].
Such complications are particularly common with long term use [7]. The reported stent-related complication rate has varied in the literature (mostly 40-60%, and as high as 87% at 20 months), based on the study population and the types/material of airway stents deployed [5].
Stents can be successfully removed endoscopically if complications arise, but the longer a metallic stent is in place, the more difficult it is to remove [8]. In this case, the stent had been in place for more than 2 years and surgical removal would have been very difficult.
In this patient, tracheostomy could not have been done and interventional tracheal therapy was required. This was to firstly remove the granulation tissue caused by the metallic stent and thereby improve the airway and secondly to obtain a histopathological diagnosis so as to determine whether the obstruction was due to granulation tissue or recurrent malignancy.
Laryngeal mask airway (LMA) or classical intubation is often used to ventilate patients with central airway obstruction. However, it usually fails to maintain oxygenation in settings where it is difficult to ventilate the patient due to significant narrowing. Venovenous extracorporeal membrane oxygenation (VV-ECMO) should be considered as a useful ventilation strategy to ensure sufficient gas exchange during the tracheal procedure in this setting. VV-ECMO entails drainage of blood from the femoral vein and the return of oxygenated venous blood to the right atrium through the internal jugular vein. It can help the patient tolerate the tracheal procedure until the resolution of severe stenosis. ECMO can not only help maintain satisfactory oxygenation during an operation, but also facilitate a better operation field. This confers a distinct advantage compared with traditional artificial airway devices [9].
Without endoscopic visualisation, airway manipulation in patients with tracheobronchial stents in situ can be catastrophic and this has been published in case reports [3].Therefore by using VV-ECMO, in this patient we were able to perform satisfactory airway evaluation, biopsy of mass at upper and lower end of tracheal stent using a rigid bronchoscope with Hopkins telescope and optical forceps and KTP laser assisted excision of granulation tissue with full endoscopic visualisation and without any complications.
Learning Points/ Take Home Messages
• Granulation tissue is the most common complication with the usage of metallic tracheal stents and can result in airway obstruction. If this complication occurs, treatment is required to remove the granulation tissue and thereby improve the airway and secondly to obtain a histopathological diagnosis so as to determine whether the obstruction is due to granulation tissue or recurrent malignancy
• Interventional tracheal therapy is a challenge in patients with metallic tracheal stents in situ
• Without endoscopic visualisation, airway manipulation in patients with tracheobronchial stents in situ can be catastrophic
• Venovenous extracorporeal membrane oxygenation (VV-ECMO) should be considered as a useful ventilation strategy to ensure sufficient gas exchange during the tracheal procedure in this setting
• By using VV-ECMO, in this patient we have shown that is possible to perform satisfactory airway evaluation, biopsy and excision of granulation tissue with full endoscopic visualisation and without any complications
Patients Perspective
“I was taken into care by the ENT surgeon and his team when I came to them complaining about breathing difficulty. Due to his immense knowledge and precise tests we were able to understand that the issue is due to the granulation tissue built surrounding my trachea. Considering the complications, they presented my case at their multi-disciplinary meetings to ensure the right course of action. The team was kind, patient and responsive to our questions and doubts regarding the subject. They were incredibly thoughtful, and compassionate and made sure I went through the procedure with confidence and positivity. It’s been three months down the line and I feel very comfortable and have shown no symptoms since. I look forward to meeting with them for follow up tests (only to hear that everything is normal and nothing less)”
References
- Sosa AF, Michaud GC. (2013) Metallic stents in the airway: should we continue to use them and can we remove them? Curr Respir Care Rep. 2: 54-60. [Ref.]
- Ko P, Liu CJ, Wu YY, Chao YC, Hsieh MK, et al. (2009) Granulation formation following tracheal stenosis stenting: influence of stent position. The Laryngoscope. 119(12): 2331-2336. [Ref.]
- Bansal S, Dhingra S, Ghai B, Gupta AK. (2012) Metallic stents for proximal tracheal stenosis: is it worth the risk? Case reports in otolaryngology. 2012: 450304. [Ref.]
- Agrafiotis M, Siempos II, Falagas ME. (2009) Infections related to airway stenting: a systematic review. Respiration; international review of thoracic diseases. 78(1): 69-74. [PubMed.]
- Lee H, Labaki WJ, Yu D, Salwen H, Gilbert CB, et al. (2017) Schneider A Ortiz R Feller-Kopman D Arias S & Yarmus L. Airway stent complications: the role of follow-up bronchoscopy as a surveillance method. Journal of thoracic disease. 9(11): 4651-4659. [Ref.]
- Davis BN, Madden AP, Sheth AJ. (2006) Crerar-Gilbert Airway management of patients with tracheobronchial stents BJA: British Journal of Anaesthesia. 96(1): 132-135. [PubMed.]
- Dialani V, Ernst A, Sun M, Lee KS, Feller-Kopman D, et al. (2008) MDCT Detection of Airway Stent Complications: Comparison with Bronchoscopy. Diana Litmanovich Alexander Bankier and Phillip M. Boiselle American Journal of Roentgenology. 191(5): 1576-1580. [PubMed.]
- Zakaluzny S, Lane JA, Mair E. et al. (2003) Complications of tracheobronchial airway stents. Otolaryngology-head and neck surgery: official journal of American Academy of Otolaryngology-Head and Neck Surgery. 128(4): 478-488. [Ref.]
- Liang Y, Zhu J, Zheng X, Qiao Q, Guan Y, et al. (2021) Application of extracorporeal membrane oxygenation in the endoscopic treatment of severe benign airway stenosis: A case report and literature review. 4(2): 48-52. [Ref.]