>Corresponding Author : Endalkachew Mekonnen Assefa
>Article Type : Case Report
>Volume : 2 | Issue : 2
>Received Date : 12 June, 2022
>Accepted Date : 22 June, 2022
>Published Date : 25 June, 2022
>DOI : https://doi.org/10.54289/JCRMH2200106
>Citation : Assefa EM, Bisetegn MS. (2022) Rupture of Rudimentary Horn Pregnancy at 16 Weeks of Gestation. J Case Rep Med Hist. 2(2): doi https://doi.org/10.54289/JCRMH2200106
>Copyright : © 2022 Assefa EM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
Addis Abeba University-College of Health Sciences-School of Medicine- department of obstetrics and gynecology
*Corresponding author: Endalkachew Mekonnen Assefa, Addis Abeba University-College of Health Sciences-School of Medicine- department of obstetrics and gynecology
Abstract
Rudimentary horn pregnancy is rare but a life-threatening complication. It usually diagnosed during second trimester after it ruptured. Early diagnosis and management may decrease the morbidity and mortality associated with it. This case report strengthens the diagnosis and management challenges and difficulties on a rudimentary horn pregnancy. An emergency laparotomy was performed and ruptured left rudimentary horn pregnancy was diagnosed. The patient transfused blood products and discharged after third post-operative days.
Introduction
Müllerian abnormalities are infrequently encountered and resulted from abnormal fusion or failure of absorption of Mullerian ducts (paramesonephric ducts) in-utero. The prevalence of congenital uterine anomalies among fertile women is reported as 1:200 to 1:600, whereas that of unicornuate uterus with rudimentary horn is even rare (> 1 in 100,000) [1].
Unicornuate uterus is caused by the non-development of the Mullerian duct; usually associated with various degrees of rudimentary horn which may be communicating or non-communicating with the cavity of the uterus. Pregnancy in the rudimentary horn is rare and represents a form of ectopic gestation, with a reported incidence of one in 76,000 to one in 140,000 pregnancies [2]. Because of the variable muscular constitution of the rudimentary horn; pregnancy can be accommodated up to varying gestation in different women. It often presents as a rupture of the uterine wall in the second trimester, manifesting as acute abdominal pain with intraperitoneal hemorrhage, with a high risk of maternal morbidity and mortality [1,2].
We report the case of a ruptured left rudimentary horn pregnancy at 16 weeks of gestation with initially consideration of abdominal ectopic pregnancy.
Case Report
A 24 years old Primigravida lady who stated to be amenorrhoic for the past 5 months, gestational age was 16wk + 6 days by ultrasound femur length (FL) measurement on the date of arrival. She presented with complains of lower abdominal pain of one week duration. She also experienced vaginal discharge, easy fatigability, tinnitus, vertigo, light headiness, urinary frequency and urgency of week duration.
She attended up to grade 8 and works as a housemaid. She was unaware of her pregnancy and didn’t start antenatal care follow up. She is sexually active and has a boy-friend. She has no history of medical, surgical and gynecology history. She has no history of vaginal bleeding, fever, chills.
Upon physical examination she was acutely sick looking (in pain), blood pressure measured as 75/35mmHg with pulse rate of 108-118 beats per minute and RR of 24. She has pale conjuctiva and dry buccal mucosa. On abdominal examination; There were a 20 weeks sized gravid uterus with negative FHB, superficial and deep tenderness on palpation and, positive for fluid-trill and shifting dullness. On pelvic assessment cervix was closed, deviated to the right side, there was cervical motion and adnexal tenderness and posterior cul-de-sac was bulged. Her hemoglobin was 7.2g/dl and trans-abdominal ultrasound showed singleton pregnancy with negative cardiac activity which measures 16 weeks and 6 days from femur length (FL) and placenta was fundal (fig.1). There was7*8 cm hyper- echoic mass in the lower pole of fetus with internal flow near to the bladder. There was also another mass seen on the right side origin can’t be ascertained it seems empty uterus and hemoperitoneum in the cul-de-sac, paracolic gutters and
Morrison’s pouch (fig.2). Uterus has normal size, homogenous myometrium with normal endometrium (fig. 3). With the impression of acute abdomen due to ruptured abdominal ectopic pregnancy resuscitation was started with crystalloid and blood products prepared.
After getting written informed consent, laparotomy was done through midline abdominal incision. The findings were: around 02 liters hemoperitonium, fetus within intact gestational sac and placenta in the abdominal cavity (fig 4). Unicornuate uterus with communicating rudimentary horn on the body at left lateral side which was ruptured and has active bleeding, healthy looking tubes and ovaries. Left ruptured rudimentary horn was removed with ipsilateral tube (fig.5). Bilateral kidney was checked intra-operatively. She was transfused with six units of whole blood and packed red blood cells. Her post-operative course was uneventful. She had one visit on eleventh post-operative day and uneventful.

Figure 1: Ultrasound picture-fetus with negative fetal heartbeat-femur length = 16weeks + 6 days

Figure 2: fetal head, mass, placenta.

Figure 3: fetal head, mass, placenta.
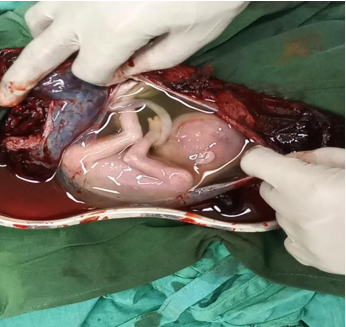
Figure 4: fetus inside gestational sac, placenta.
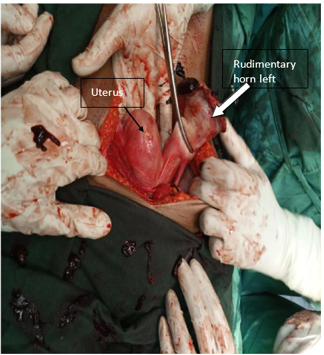
Figure 5: Intraop – uterus, left rudimentary horn.
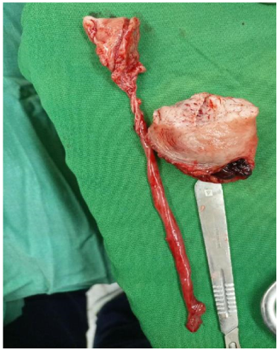
Figure 6: Left fallopian tube, cut part of rudimentary horn.
Discussion:
A unicornuate uterus represents 4%-5% of uterine abnormalities and is further classified into 4 categories:
(1) communicating, cavitary, rudimentary horn,
(2) non-communicating cavitary, rudimentary horn
(3) non-cavitary rudimentary horn
(4) Unicornuate uterus without a rudimentary horn,
which is that the most typical form. Over half of the rudimentary horns comprise a cavity with functional endometrium, and 72%-80% of them are non-communicating and right-sided [3,4,5].
Early diagnosis of a rudimentary horn pregnancy is difficult. The most significant danger of rudimentary horn pregnancy is that the risk of rupture due to poorly developed musculature [5]. 80%-90% of rudimentary horn pregnancies rupture between the 10th and 15th weeks of gestation and also the majority of the cases are detected after rupturing of the horn, which might have grave consequences for both mother and fetus [6]. Correct ultrasound diagnosis of asymptomatic cases occurs in only 8% of the cases, while most are diagnosed intra-operatively when symptoms occur [4]. Abdominal pain and collapse with hemoperitoneum can occur suddenly [5]. Pelvic examination may suggest an adnexal mass, causing deviation of the uterus and cervix to one side [7].
Tsafrir proposes 3 fundamental criteria on ultrasound for the ultimate diagnosis of pregnancy in a rudimentary horn, which are: pseudo-pattern of an asymmetrical bicornuate uterus; absent visual continuity between the cervical canal and the lumen of the pregnant horn; the presence of myometrial tissue surrounding the gestational sac [8].
Removal of the rudimentary horn and also the ipsilateral tube through either laparotomy or laparoscopy is suggested because the functional endometrial horn is related to an increased risk for dysmenorrhea, infertility, or ectopic pregnancy which is that the gold standard for management at any trimester [6].
Even though the patient presented late, there was clinical finding like deviated cervix on pelvic examination and ultrasound finding of empty uterus suggesting müllerian anomaly but it was not considered differential. Obstetricians and radiological professionals must maintain a high degree of suspicion to prevent the morbidity associated with this condition [3,8].
Patient consent
Written, informed consent of this case was obtained from the patient.
Conflicts of interest
The authors declare that they have no conflicts of interest.
References
- Heinonen PK, Saarikoski S, Pystynen P. (1982) Reproductive performance of women with uterine anomalies. Acta Obstet Gynecol Scand. 61: 157-162. [PubMed.]
- Johansen K. (1983) Pregnancy in a rudimentary horn. Obstet Gynecol. 61: 565-567. [Ref.]
- Nahum GG. (2002) Rudimentary uterine horn pregnancy. The 20th-century worldwide experience of 588 cases. J Reprod Med. 47(2): 151-163. [Ref.]
- Khati NJ, Frazier AA, Brindle KA. (2012) The unicornuate uterus and its variants: clinical presentation, imaging findings, and associated complications. J Ultrasound Med. 31(2): 319-331. [PubMed.]
- Jayasinghe Y, Rane A, Stalewski H, Grover S. (2005) The presentation and early diagnosis of the rudimentary uterine horn. Obstet Gynecol. 105(6): 1456-1467. [PubMed.]
- Siwatch S, Mehra R, Pandher DK, Huria A. (2013) Rudimentary horn pregnancy: a 10-year experience and review of literature. Arch Gynecol Obstet. 287(4): 687-695. [PubMed.]
- Wahlen T. (1972) Pregnancy in non-communicating rudimentary uterine horn. Acta Obstet Gynecol Scand. 51: 155-160. [Ref.]
- Tsafrir A, Rojansky N, Sela HY, Gomori JM, Nadjari M. (2005) Rudimentary horn pregnancy: first-trimester prerupture sonographic diagnosis and confirmation by magnetic resonance imaging. J Ultrasound Med. 24(2): 219-223. [PubMed.]