>Corresponding Author : Gandhi Ranju
>Article Type : Case Report
>Volume : 2 | Issue : 3
>Received Date : 27 Sep, 2022
>Accepted Date : 07 Oct, 2022
>Published Date : 10 Oct, 2022
>DOI : https://doi.org/10.54289/JAAD2200111
>Citation : Prerana J, Ranju G, Anoop G and Rahul K. (2022) Anaesthetic Management of a Case of Vanishing Lung Syndrome Undergoing Cholecystectomy. J Anaesth Anesth Drug 2(3): doi https://doi.org/10.54289/JAAD2200111
>Copyright : © 2022 Prerana J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Senior resident, VMMC and Safdarjung Hospital, New Delhi
2Professor, VMMC and Safdarjung Hospital, New Delhi
3Postgraduate student, VMMC and Safdarjung Hospital, New Delhi
*Corresponding author: Gandhi Ranju, Professor, VMMC and Safdarjung Hospital, New Delhi
Abstract
Vanishing lung syndrome is a rare radiological syndrome in which the lungs appear to be disappearing on x- ray due to giant bulla. Anaesthetic considerations in a patient with bullous lung disease undergoing a non-thoracic surgery are to prevent enlargement and rupture of bulla causing pneumothorax and maintaining adequate oxygenation and ventilation.
We present a case of 62-year-old female with vanishing lung syndrome posted for cholecystectomy for symptomatic gall bladder stones. We decided to proceed with open cholecystectomy instead of laparoscopic procedure in view of giant bulla and severely impaired lung functions. Our plan of anaesthesia for open cholecystectomy was combined spinal and epidural anaesthesia which allowed us to avoid positive pressure ventilation, nitrous oxide, high airway pressures, coughing at extubation and sore throat concerns.
Keywords: vanishing lung syndrome, giant bulla, pneumothorax
Abbreviations: PFT: Pulmonary Function Test
Introduction
Vanishing lung syndrome is a rare radiological syndrome in which the lungs appear to be disappearing on x- ray due to large bulla [1-3]. Patient presenting with vanishing lung syndrome for a non-thoracic surgery is rare [4]. Anaesthetic management of a patient with giant bulla covering more than 2/3rd of the hemithorax for open cholecystectomy requires special consideration.
Case Presentation
We present a case of 62-year-old female with vanishing lung syndrome posted for cholecystectomy for symptomatic gall bladder stones.
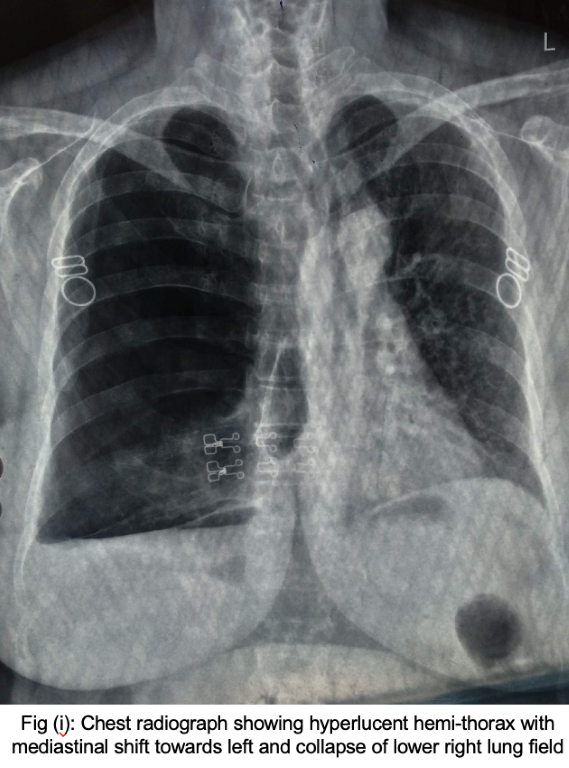
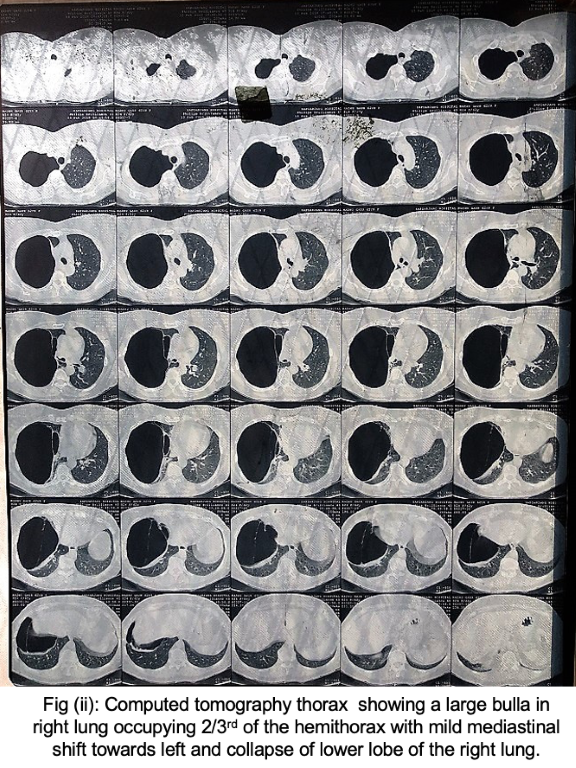
The patient was a non- smoker with no other systemic co-morbidities. She had complaint of breathlessness on moderate exertion and her metabolic equivalent was 4. On respiratory examination, decreased air entry was found on right side of the chest. Examination of other systems was normal. Her haematological and biochemical investigations, electrocardiogram and echocardiogram were normal. Chest x-ray showed radiolucency and absence of lung marking on the right side of the chest. Computed tomography thorax (fig.1) showed a large bulla in right lung with intervening septa occupying 2/3rd of the hemithorax with mild mediastinal shift towards left and collapse of lower lobe of the right lung. Pulmonary function test (PFT) showed FEV1 50% of predicted, FVC 58% of predicted and PEFR 66% of predicted value indicating severe airflow limitation. Her room air saturation was 94% and arterial blood gas on room air showed a pH of 7.44, pO2 of 81.5, pCO2 of 33.4, HCO3 of 24.4 and sO2 of 95.6%.
The case was discussed with the surgeon and pulmonologist, and it was decided to proceed with open cholecystectomy instead of laparoscopic cholecystectomy in view to giant bulla and severely impaired pulmonary functions. Preoperatively, the patient’s respiratory functions were optimized with formoterol, budecort and levosalbutamol metered dose inhalers. Our plan of anesthesia for open cholecystectomy was combined spinal and epidural anesthesia. Patient was kept nil per oral for 8 hours before surgery and given tablet ranitidine 150 mg night before the surgery and in the morning. High risk consent and ICU bed was made available. On the day of surgery, the patient received nebulisation with ipratropium bromide and levosalbutamol. Appropriately sized chest drain tube, metered dose inhalers and all necessary emergency resuscitation drugs were kept ready. On arrival to the operation theatre, all standard ASA monitors (electrocardiogram, non invasive blood pressure, pulse oximetry and skin temperature) were applied. Intravenous 18G cannula was secured and patient was coloaded with 500 ml of Ringer lactate. Under aseptic precautions, in sitting position (fig.2), skin infiltration was done with 2% lignocaine and L2-L3 epidural space was identified with 18 G Tuohy’s needle at 3.5 cm from skin. Spinal anesthesia was given with 27 G spinal needle by needle through needle technique with bupivacaine heavy (0.5%) 2.4 ml and 15 mcg fentanyl. Epidural catheter of size 20 G was threaded. Sensory level of block was T4 and motor block was grade IV by modified bromage scale. Intavenous paracetamol 1 gram infusion and morphine 3 mg was given for multimodal analgesia. Intravenous promethazine 15 mg and ondensetron 4 mg was given for anti- emesis. The surgery lasted for 90 minutes. Intraoperatively, patient remained haemodynamically stable and pain free. Patient was shifted to the recovery room where level of block and pain score was checked every 15 minutes. The level of block receded to T8 after 2 hours and then morphine 1.5 mg in 5 ml saline was given through epidural catheter. Epidural catheter left in situ to provide postoperative analgesia and also to manage any surgical reexploration issues.
Patient was shifted to high dependency unit. Intravenous paracetamol 1 gram infusion and epidural bupivacaine (0.125%) 5 ml was given when VAS score for pain was 5/10. Epidural catheter was removed on next morning. The patient was then maintained on intravenous paracetamol 8 hourly. She was discharged on 4th postoperative day.
Discussion
Bulla is dilated air space in the lung parenchyma more than one cm. When the bulla occupies more than 30% of the hemithorax, it is termed as giant bulla [3]. Most common cause of giant bulla is chronic obstructive pulmonary disease. Other causes include α1- antitrypsin deficiency, Marfan’s syndrome, Ehler- Danlos syndrome, cocaine smoking and sarcodiosis [5].
Giant bulla increases the physiological dead space and compresses the surrounding normal lung tissue [1]. It can further exert pressure on diaphragm. Enlargement of bulla can cause worsening of ventilation. This can further be complicated by spontaneous rupture causing pneumothorax, bulla infection and haemorrhage into the bulla.
Asymptomatic bullae are treated conservatively by reassurance, advice to stop smoking and avoiding sternous activities that can promote rupture of bulla. Surgery is indicated for the patients who have incapacitating dyspnea or who have complication related to bullous disease [4,6].
Patients should undergo CT scan and PFT for preoperative evaluation to assess the extent of the bullous disease and the quality of the surrounding lung tissue. Smoking cessation and outpatient pulmonary rehabilitation are required for all patients preoperatively [4].
Anaesthetic considerations in a patient with bullous lung disease undergoing a non-thoracic surgery are to prevent enlargement and rupture of bulla causing pneumothorax and maintaining adequate oxygenation and ventilation [7].
Pneumothorax can be best prevented by avoiding positive pressure ventilation, if the type of surgery permits. Positive pressure ventilation should include keeping minimum airway pressure and avoiding nitrous oxide which can further expand the air filled spaces [7,8].
Prevention of postoperative sore throat due to high cuff pressure can prevent coughing and bucking and hence undue stress on the pulmonary bullae.
Laparoscopic procedure is a further threat as increase in intraabdominal pressure can further hamper the ventilation [8]. Keeping minimal intraabdominal pressure should be considered in laparoscopic surgeries.
Moreover, immediate availability of chest drain and emergency drugs in operation theatre is important. Meticulous monitoring is required to urgently detect any adverse consequences.
Conclusion
Anaesthetic management in a case of vanishing lung syndrome should include adequate preoperative work up and accordingly proper preparation of the patient. Avoidance of positive pressure ventilation, nitrous oxide, high intraabdominal pressure and preparation for adverse consequences are the key factors for safe outcome in a patient with giant bulla.
Conflicts of interest: Nil
References:
- Vij AS, James R, et al. (2014) A rare case of vanishing lung Syndrome. J Assoc Physicians India. 62(12): 51-53. [PubMed.]
- Hassan G, Javid A, et al. (2001) Vanishing Lung Syndrome. JK- Practitioner. 8(1): 248-249. [Ref.]
- Stern EJ, Webb WR, Weinacker A, et al. (1994) Idiopathic giant bullous emphysema (Vanishing lung syndrome): Imaging findings in nine patients. AJR Am J Roentgenol. 162: 279-282. [PubMed.]
- Greenberg JA, Singhal S, Kaisen LR. (2003) Giant bullous lung disease: Evaluation, selection, techniques and outcome. Crest Surg Clin N Am. 13(4): 631-649. [PubMed.]
- Henao-Martinez AF, Farnandez JF, Adams SG, Restrepo C. (2012) Lung bullaewith air fluid levels: what is the appropriate therapeutic approach? Respi Care. 57(4): 642-645. [Ref.]
- Bael VK, Meir ML, Vanoverbeke H. (2014) Video- assisted Thoracoscopic Resection of a Giant Bulla in Vanishing Lung Syndrome: case report and a short literature review. J Cardiothoracic Surg. 9: 4. [Ref.]
- Mottaghi K, Asadi S, Safari F, Nashibi M. (2016) Anesthesia Management of Bullous Emphysema in Patient Candidate for craniotomy. Ann Anesthesiology Crit Care. 1(1): e10190. [Ref.]
- Dutta B, Gangaprasad. (2012) Anaesthetic Management of a Case of Giant Pulmonary Bulla Undergoing Laparoscopic Cholecystectomy. JAnesth Clin Res. 3: 214. [Ref.]